What are mid-urethral slings?
Mid-urethral sling (also known as tape) procedures are operations designed to help women with stress incontinence. Stress incontinence is the leakage of urine with everyday activities such as coughing, sneezing, or exercise. It is a very common and embarrassing problem affecting up to 1 in 3 women. Stress incontinence may be cured or improved with pelvic floor exercises and lifestyle modifications, but if these strategies fail, then surgery may be recommended. The most frequently offered type of operation is a mid-urethral sling procedure, a simple day case procedure that has been performed for more than 3 million women worldwide.
The operation involves placing a sling of polypropylene mesh (suture material that is woven together – about 1 cm wide) between the middle portion of the urethra and the skin of the vagina. The urethra is the pipe through which the bladder empties. Normally the muscle and ligaments which support the urethra close firmly when straining or exercising to prevent leakage. Damage or weakening of these structures by childbirth and/or the aging process can result in this mechanism failing, leading to urine leakage. Placing a sling underneath the urethra improves the support and reduces or stops leaking. Mesh sling procedures have been done safely for many years, however, in view of the recent media coverage of vaginal meshes, we have provided answers to frequently asked questions about meshes on our website.
How is a sling performed?
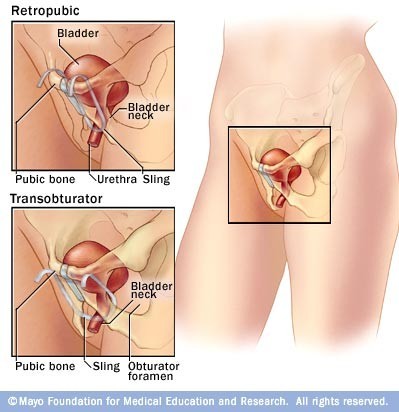
There are three main routes for placing the sling: The retropubic route, the transobturator route, and the “single incision” or “minisling.”. In some women with severe stress incontinence the retropubic route appears to be more successful. Mini-slings are less invasive than the other methods but are not quite as effective in controlling stress incontinence in the longer term or in women with severe incontinence. The surgical route will depend on your doctor and the common practice in your part of the world.
Retropubic Route
In the retropubic approach, the sling is placed through a small cut made in the vagina over the mid-point of the urethra. Through this the two ends of the sling are passed from the vagina, passing either side of the urethra, to exit through two small cuts made just above the pubic bone in the hairline, about 4-6 cm apart. The surgeon will then use a camera (cystoscope) to check that the sling is correctly positioned and not sitting within the bladder. The sling is then adjusted so that it sits loosely underneath the urethra and the vaginal cut is stitched to cover the sling over. The ends of the sling are cut off and they too are covered over. The most common retropubic operation to be carried out is the TVT (Tension-free Vaginal Tape). This is also the operation that has been done for the longest time, and research suggests that if it is initially successful in controlling stress incontinence then it is still likely to be working up to at least 17 years later. The other retropubic procedures are likely to have similar long-term success rates.
Transobturator Route
In the transobturator approach, a small incision is made in the vagina at the same place as for the retropubic operation. The ends of the sling are passed through two small incisions made in the groin. Each end of the sling passes through the obturator foramen, which is a gap between the bones of the pelvis. The ends are cut off once the sling is confirmed to be in the correct position and the skin closed over them.
Mini-sling
The mini-sling procedure is similar to the initial part of the retropubic approach, except that the ends of the sling do not come out onto the skin and are anchored in position.
How does a sling work?
The sling (or tape) prevents leakage by supporting the urethra and mimicking the ligaments that have been weakened by having babies and the aging process. Once the sling is in position, tissue grows through the holes in the weave and so anchors the sling in position. This may take 3 to 4 weeks.
Does a sling require anesthesia?
Although it is possible to do the operation with just local anesthetic, most surgeons would supplement this with a strong sedative or full general anesthesia. Occasionally, the operation is done using a spinal or an epidural anesthetic.
What are the chances that the sling will fix my problem?
Research tells us that, in the short term, this operation is as successful as other more invasive procedures used for controlling stress incontinence, but with a quicker recovery and less chance of needing surgery for prolapse in the first two years after the surgery. Between 80-90% of women are happy with their operation and feel that their incontinence is either cured or much better. However, there are a small number of women for whom the operation does not seem to work. The operation is less likely to be a success if you have had previous surgery to your bladder (such as a repair operation).
Are there other options to manage my incontinence?
• Pelvic floor exercises (PFE). Pelvic floor exercises can be a very effective way of improving symptoms of stress urinary incontinence. Up to 75% of women show an improvement in leakage reduction after PFE training. The benefits of pelvic floor exercises are maximized if practice is carried out regularly. Maximum benefit usually occurs after 3 to 6 months of regular exercising. You may be referred to a physical therapist (physiotherapist) to supervise this. If you also have a problem with urge urinary incontinence your doctor may also advise bladder retraining exercises.
• Continence devices. Continence devices are available which fit in the vagina and help control leakage. These can be inserted prior to exercise or worn continuously. Some women find inserting a large tampon prior to exercise may prevent or reduce leakage. These types of devices are most suitable for women with more minor degrees or urinary incontinence or who are waiting definitive surgical treatment.
• Lifestyle changes. If you are overweight, reducing weight can result in an improvement in incontinence symptoms. Maintaining good general health, quitting smoking, and having good control of medical conditions such as asthma can also be helpful.
