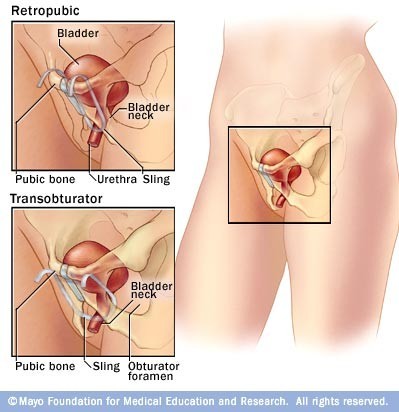
You are considering or are scheduled for a surgical procedure called a vaginal or mid-urethral sling. The purpose of this procedure is to create a hammock of support and to prevent the urethra from opening when you cough, laugh, or sneeze. The procedure involves placing a piece of synthetic mesh (polypropylene mesh) under the urethra. Depending on your particular symptoms and preference, the procedure can be performed in one of two ways: just above the vagina on the lower abdomen (retropubic) or into the groin creases (transobturator technique). Through a vaginal incision, a strip of mesh is positioned under the urethra to create a supportive sling and to reduce or even eliminate urinary incontinence.
DO NOT TAKE ASPIRIN, BLOOD THINNING MEDICATIONS, VITAMINS AND HERBAL SUPPLEMENTS FOR 1 WEEK PRIOR TO SURGERY.
This includes Coumadin, Heparin, Motrin®; Advil®, ibuprofen, Aleve®; glucosamine; vitamins A, C, D, and E; garlic; Echinacea; and omega-3 fatty acids. If necessary you can safely take Tylenol® for headaches or pain. Any other medication such as antibiotics, high blood pressure pills, and heart medications should be continued unless otherwise specified. Please discuss any concerns about stopping these medications with your family doctor.
DIABETICS: If you take NPH insulin, you should take ½ the regular dose the night before surgery but DO NOT take any NPH the morning of surgery.
DO NOT EAT OR DRINK ANYTHING AFTER 12 MIDNIGHT THE DAY BEFORE SURGERY. Any medications that must be taken the morning of surgery should be taken with a small sip of water.
What does surgery entail?
Vaginal sling procedures are almost exclusively done on an outpatient basis. However in special cases we may keep you for 23 hours in the hospital or an ambulatory surgery center. The procedures are done almost entirely through the vagina. A small incision is necessary just above the hairline or in the thigh creases for placement of some sutures or the mesh. Due to the small size of the incision and dissection, there is less discomfort and more rapid recovery in comparison to previous surgical treatments. We use absorbable sutures in the vagina which will dissolve in a few weeks. The retropubic sling requires sutures or bandages just above the hairline as well.
What are the risks and complications of the vaginal sling procedure?
Complications following this type of procedure are rare in the hands of surgeons with specific advanced training. The most common complications include bleeding and infection, injury to surrounding structures, pain, urinary retention (inability to urinate), recurrent or worsening incontinence, urgency or urge type incontinence. As outlined in the FDA article, erosions and infections of the graft material have been reported. These were predominantly associated with a specific type of mesh which has been removed from the market However, the risk still remains and this should be addressed with your surgeon at the time of consultation.
What happens after surgery?
Following surgery, your vagina will be packed for about 1 hour with a gauze roll in order to minimize bleeding. You may have a catheter exiting the urethra, although some patients can successfully void in the recovery area, and leave without a catheter. You will be given instructions on removing your catheter the morning after surgery (at home), if it is determined that you should be discharged with the catheter. The catheters are in place to allow you to empty your bladder, as there is swelling after surgery that often prevents this or makes it difficult. After the swelling subsides, you will gradually be able to urinate. Your normal pattern may not return for a few weeks, but this is normal in the course of events and not cause for alarm.
The most important development has been the use of synthetic slings placed at the middle portion of the urethra, termed “mid-urethral slings.” These operations have primarily been used for SUI patients who have loss of urethral support or urethral hypermobilty. These midurethral slings are placed loosely and appear less likely to cause problems with urination. Although synthetic materials had been used in the past, the complication rate, primarily urinary tract infection and erosion (also tissue ulceration, breakdown, or irritation) was unacceptably high. Newer materials and a needle approach through the skin with minimal cutting, along with “tension-free” placement in the mid-urethra, have led to these operations becoming the most popular procedures in the United States and Europe. The TVT (tensionfree vaginal tape) has been performed for over 15 years, and an impressive number of reports attest to the 10-year effectiveness. Because the sling is made of permanent, synthetic material, there is evidence that the long-term results are also good.
The primary question relates to the very long-term safety of permanent material around the urinary tract and the risk of erosion into the bladder or urethra many years down the road.
Like all surgeries for stress incontinence, the mid-urethral sling is not as effective when patients have had prior surgery. A high quality study demonstrated equal effectiveness to the Burch procedure (the former “gold standard” procedure) at six months and superior results at 5 and 10 years. The TVTtype procedures are usually easier for the patient, generally performed as an outpatient with a general anesthesia, or sometimes under sedation with local anesthesia. There are now a number of competitive products offering slightly different sling material and/or methods of placement. While a very popular and effective procedure, the route used to deliver the TVT sling does not allow surgeons a full view of the pelvic organs. One increasingly popular technique is a transobturator (TOT) approach that uses a different incision site considered to lower the risk of urethral and bladder injury. There are still other techniques that deliver synthetic slings, which are either meant to lower injury risk and/or achieve greater compression of the urethra.
